Conditions Treated
List of Conditions
The goal with our therapies is to address symptoms, reduce or mitigate pain and get the the bottom of the sources. In this way we strive to get you back to an active life. Here is a list of some common conditions and injuries we treat:
| Achilles Tendon | Muscle Spasms |
| ACL Tear or Strain | Nerve Pain |
| Arthritis / Bursitis | Osteoarthritis |
| Back Pain | Osteoporosis |
| Carpal Tunnel | Parkinson’s Disease |
| Cellulite/Fat Reduction | Peripheral Neuropathy |
| Fatigue | Plantar Fasciitis |
| Fibromyalgia | Post- Surgical Pain |
| Golfer’s Injuries | Scar Release/Reduce |
| Hair Loss | Sciatica |
| Hamstring Pull | Shingles |
| Herniated Discs | Sports Injuries |
| Inflammatory Issues | Sprains or Strains |
| Knee Pain | Tennis Elbow |
| Lymphedema | TMJ |
| Migraines | Toe Fungus |
| Wounds |
Auto Accident
If you have been in an auto accident, the sooner you seek treatment the better your chances for a full recovery. Due to adrenaline after an auto accident you may not feel symptoms right away, so seek medical help anyway.
Common Injuries include:
- Whiplash
- Upper Back Pain
- Mid Back Pain
- Low Back Pain
- Sciatica
- Radiating Arm Pain
- Radiating Leg Pain
- Muscle Aches
- Tingling/numbness in arms and legs
Back and Neck Injuries
Any neck or back injury could cause a victim significant pain and suffering, a temporary disability, and lost wages.

Whiplash is the most common injury when rear ended.
Rear-end crashes are the most frequently occurring type of collision, accounting for approximately 29% of all crashes. (NHTSA, 2017)
Pain areas: in the neck, arm, back, muscles, or shoulder
Whole body: dizziness or vertigo
Also common: difficulty focusing, headache, muscle spasms, nerve injury, sensation of pins and needles, sleep disorder, stiff neck, or tenderness
Worker's Compensation
When you are injured on the job, all you want to do is get back to work as soon as possible. That’s why our clinic receives frequent referrals from insurance companies for treatment. Here are some frequently asked questions injured Florda workers often have:
HOW LONG AFTER AN ACCIDENT DO I HAVE TO REPORT IT TO MY EMPLOYER?
You should report it as soon as possible but no later than thirty (30) days or your claim may be denied.
WHAT KIND OF MEDICAL TREATMENT CAN I GET?
The medical provider, authorized by your employer or the insurance company, will provide the necessary medical care, treatment and prescriptions related to your injury
IF I AM UNABLE TO RETURN TO WORK UNTIL MY DOCTOR RELEASES ME, DOES MY EMPLOYER HAVE TO HOLD MY JOB FOR ME?
No, there is no provision in the law that requires your employer to hold the job open for you
Sports Injuries
Achilles tendon injuries. Your Achilles tendon is the thick, corded tissue that connects your calf muscle (in the back of your lower leg) to your heel. This is the largest tendon in your body. It’s used to help you walk. Achilles tendinitis is a common injury to the Achilles tendon. It’s common in sports that require a lot of running. It can be caused by not stretching enough before playing, not wearing the right shoes, or suddenly playing the sports more. You may have Achilles tendinitis if your heel or calf hurts when you walk or run. Other symptoms include swelling in the area or if the area is warm to the touch. These injuries can be both acute or chronic.
Broken bones. A broken bone is caused by sudden force being applied to a bone. This is sometimes also called a fractured bone. This can happen in almost any sport. Symptoms include sudden pain, swelling, numbness, and tenderness around the area. You may notice the affected area doesn’t look right and you may not be able to move it. These injuries are acute.
Dislocations. It’s sometimes hard to tell the difference between a broken bone and a dislocation. A dislocation happens when the ends of your bones move out of their normal position. These are common in contact sports, such as football, soccer, and basketball. Symptoms include extreme pain, swelling, and not being able to move the area. These injuries are acute.
Jumper’s knee. This is also known as patellar tendinitis. Jumper’s knee happens when there is an injury (or inflammation) to the tissue that connects your kneecap and thigh muscles your shin bone. Sports with repetitive jumping are common triggers for this injury. Examples include basketball and volleyball. Also, people who are overweight or play sports on a hard surface are more likely to get jumper’s knee. Symptoms include knee pain, usually just below the kneecap. You may experience weakness or stiffness in the knee while jumping, kneeling, or climbing stairs. These injuries can be both acute or chronic.

Rotator cuff injuries. Your rotator cuff is an area inside your shoulder. It helps your shoulder move and keeps it stable. Injuries to this area are common when the same actions are repeated many times, such as in swimming, tennis, or baseball. Symptoms include swelling in your shoulder, pain when you lift your arm, and pain when you try to reach behind your back. This injury is chronic.
Runner’s knee. Runner’s knee is another repetitive-motion injury. It’s common to runners and anyone who does a lot of walking, biking, or general knee bending. It can also be caused by knee trauma or a hard bump to the knee. Symptoms include pain behind your kneecap, especially when you bend your knee. The area may be swollen, or you may feel a grinding sensation when your knee bends. These injuries can be both acute or chronic.
Shin splints. Your shin is the area at the front of your lower leg, below your knee. Shin splints happen when the muscles and tendons around your shin become inflamed. This injury often impacts runners and basketball players. The main symptom of shin splints is pain in the front of your lower leg while playing the sport. The pain usually goes away with rest. These injuries are acute.
Sprains. A sprain is one of the most common sports injuries. A sprain is a stretch or tear of a ligament near a joint, such as a knee, ankle, or wrist. Sprains are most often caused by falling or by a twisting motion. They can be mild or severe, depending on whether the ligament is stretched or torn. Symptoms are pain, swelling (sometimes severe), and bruising. You may also not be able to apply weight to the joint without pain. These injuries are acute.
Strains. A strain and a sprain are different. A strain hurts a muscle, while a sprain hurts a ligament. A strain occurs when you stretch or tear muscle tissue by overextending it. Mild strains can be caused by repetitive motion. In sports, acute strains are most likely to occur when you are running, jumping, or lifting. They also happen when you quickly change direction. You’re more likely to strain a muscle in cold weather. Symptoms are sudden pain followed by immediate limited range of motion to the affected area. In severe cases, you may also see bruising and swelling. These injuries can be chronic or acute.
Tennis elbow. Tennis elbow is a painful condition caused by overusing your elbow. Tennis players and golfers are likely to get it. It causes pain on the outside of your elbow. The pain is caused by inflammation in the tendons. Other symptoms may include weakness, especially as you try to grip objects. These injuries can be chronic.
SOURCE: American Academy of Family Physicians
Back Pain
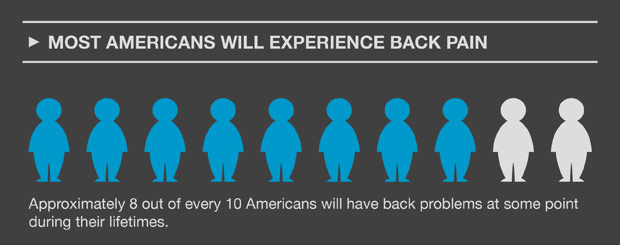
One of the most common medical problems, affecting 8 of 10 people at some point in their life.
Back pain ranges from a dull, constant ache to a sudden, sharp pain. Acute back pain comes on suddenly and lasts a few days to a few weeks. Chronic back pain lasts for more than three months.
Most back pain goes away on its own, though it may take awhile. Taking over-the-counter pain relievers and resting can help. However, staying in bed for more than 1 or 2 days can make it worse.
If your back pain is severe or doesn’t improve after three days, you should call your health care provider. You should also get medical attention if you have back pain following an injury.*
Three common classifications of back pain include:
Axial pain. Also called mechanical pain, axial pain is confined to one spot or region.
Referred pain. Often characterized as dull and achy, referred pain tends to move around and vary in intensity.
Radicular pain. Commonly described as electric shock-like or lightening pain, radicular pain travels down the spinal nerve.
Low Back Pain
Low back pain is the number two reason that Americans see their health care provider. It is second only to colds and flu. Injuries are a common cause of low back pain. Examples include a muscle strain or spasm, ligament sprain, joint problem, or a “slipped disk.” You will usually first feel back pain just after you lift a heavy object, move suddenly, sit in one position for a long time, or have an injury or accident.*
* NIH: National Institute of Arthritis and Musculoskeletal and Skin Diseases
Sciatica. Sciatica pain is caused by an irritation, inflammation, pinching or compression of a nerve in the lower back. The most common cause is a herniated or slipped disk that causes pressure on the nerve root. Pain originates in the spine and radiates down the back of the leg. Sciatica typically affects only one side of the body.
Upper Back Pain
The upper back is the area between the base of the neck and the bottom of the ribcage. There are 12 bones that make up the upper back called the thoracic spine. Less common that lower back pain, upper back pain is commonly caused by poor posture or overuse. Less common causes include traumatic injury (IE: car accident, fall), herniated disk, pinched nerve, osteoarthritis, fibromyalgia, scoliosis and more.
Peripheral Neuropathy
Loss of balance and injuries related to poor balance are a major concern.
Hip fractures, broken arms and concussions can all occur because of poor balance related to loss of foot sensation. Neuropathy can disturb your balance and that is a very serious problem.
If your feet are numb, you may be less likely to feel when they’ve become injured. Make sure to check your feet regularly so that you can treat minor injuries before they become infected. This is especially important for people with diabetes, who tend to heal more slowly.
5 Common Myths-Peripheral Neuropathy
Myth #1- Diabetes is causing your peripheral neuropathy.
Even if you have diabetes, you probably have other contributing factors. If you eat the standard diabetes diet you could be ruining your nerves.
Myth #2- You have chemotherapy related neuropathy and told to live with it.
Chemotherapy does commonly cause peripheral neuropathy but there are measures to take to help resolve pain after treatment. Some patients are told it will get better on its own, it usually does not.
Myth #3- Spinal stenosis is pinching on your nerves.
You may have spinal stenosis but once again, you most likely have other contributing factors for your peripheral neuropathy. If you work on the underlying condition, you can get better.
Myth #4- Alcohol created my neuropathy!
Well maybe, partially, but usually with alcohol you may have intrinsic factor problems and other gastrointestinal problems that allowed the alcohol to do its damage.
Myth #5- My cholesterol medication (statins) killed my nerves and muscles!
Some of the hardest cases for peripheral neuropathy to help are patients on statins. However, there is usually a root functional cause that can be found and still eliminate pain.
Symptoms of Peripheral Neuropathy
It doesn’t matter if you have diabetic, post chemotherapy or neuropathy due to an unknown cause…the rules around healing the nerves do not change.
Symptoms depend on the kind of peripheral nerves that have been damaged. Because each peripheral nerve has a specialized function in a specific part of the body, a wide array of symptoms can occur.
Some people may experience temporary numbness, tingling, and pricking sensations (paresthesia), sensitivity to touch, or muscle weakness. Others may suffer more extreme symptoms, including burning pain (especially at night), muscle weakness, paralysis, or organ or gland dysfunction.
The symptoms of peripheral neuropathy include:
- A sensation of wearing an invisible “sock”
- Burning sensation or freezing pain
- Sharp, jabbing or electric-like pain
- Extreme sensitivity to touch
- Difficulty sleeping because of feet and leg pain
- Loss of balance and coordination
- Muscle weakness, shrinking
- Difficulty walking or moving the arms
- Unusual sweating
- Problem digesting food, swallowing, feel bloated, heartburn
- Abnormalities in blood pressure or pulse
Treatments for Peripheral Neuropathy
Our program for treating Peripheral Neuropathy is a combination of procedures that incorporate fall risk testing, fall prevention activities along with with breakthrough non-invasive medical therapy.
Individualized Treatment – We will perform a thorough evaluation and develop an individualized treatment program meant to improve your quality of life.
Functional Assessment – Our trained medical staff will give you a functional assessment that will identify specific exercises to challenge your balance. We will then improve strength, flexibility and reaction time so you can quickly make adjustments when losing balance.
Modalities Utilized – Deep Tissue Laser and Nerve Root Sedation (Electroanalgesia) are paired together to relax the nerve and help manage the symptoms at the same time. Additional therapies may include platelet-rich-plasma or other natural biologic injections.
One of the most exciting parts of our program is that it has a beginning and an end … unlike the drugs you may be taking which are typically taken everyday, or more, forever. By offering proven state-of-the-art technologies, matched with innovative approaches for optimal, long-lasting results, we work together with you to help pursue a pain-free and satisfying life full of vitality.


